Case report
peer-reviewed
Published: January 15, 2023 (see history)
DOI: 10.7759/cureus.33801
Cite this nonfiction as: Yoshimura A, Kusama Y, Omura Y, et al. (January 15, 2023) A Case of Eating Disorder Diagnosed As Orthorexia Nervosa. Cureus 15(1): e33801. doi:10.7759/cureus.33801
Abstract
A 13-year-old miss presented to our infirmary with main complaints of accelerated value loss, fatigue, discomfort, chills successful the extremities, and alopecia. We initially suspected anorexia nervosa (AN). However, she did not explicit fearfulness of gaining value oregon person a distorted cognition of her value oregon assemblage shape; thus, her presumption was not emblematic of AN. We besides suspected avoidant/restrictive nutrient intake upset (ARFID), but she did not grounds immoderate food-avoidance behaviors. However, she was obsessed with nutrition control, truthful we diagnosed her with orthorexia nervosa (ON). She was hospitalized, fixed acquisition connected due nutrition, and her eating behaviour subsequently improved. After discharge, we administered the ORTO-15, which assesses the propensity for ON, and her people met the diagnostic criteria for ON. The incidence of ON has accrued during the COVID-19 pandemic. In this case, her obsession was brought astir by accusation she work successful magazines and connected societal media that promoted an unbalanced fare centered astir exclusively connected vegetables. Pediatricians should rise consciousness of misinformation regarding children’s wellness to guarantee steadfast growth.
Introduction
Mortality rates from eating disorders are 5.2-6.5 times higher successful radical with anorexia nervosa (AN), 1.4-1.5 times higher successful those with bulimia nervosa (BN), and 1.5-2.3 times higher successful those with binge eating upset compared with the same-aged colonisation [1]. Thus, physicians should admit that eating disorders tin beryllium fatal. The morbidity of eating disorders is higher successful the colonisation aged ≥10 years [2]; therefore, eating disorders bash not ever hap successful adults. Thus, pediatricians should cognize the ways to diagnose and dainty eating disorders. In 2013, the 5th variation of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) was published, and the classification of eating disorders was updated. However, the American Psychiatric Society has not yet recognized orthorexia nervosa (ON) and is truthful not included successful the DSM-5. Herein, we study a diligent with an eating upset who met the diagnostic criteria for ON.
Case Presentation
A antecedently steadfast 13-year-old Japanese miss successful inferior precocious schoolhouse with nary diagnosed developmental disablement presented to our infirmary with terrible value loss. She was quiescent and had made nary evident occupation betwixt friends and teachers during simple school. Her schoolhouse grades successful inferior precocious schoolhouse were mostly fair. She has nary siblings, and her parents did not person immoderate histories of eating disorders and were not funny successful healthism. Five months earlier the infirmary visit, she gradually began to suffer weight. Two months before, her value rapidly declined, she stopped menstruating, and hairsbreadth nonaccomplishment was noted. There were nary episodes of overeating, nary self-induced vomiting, nary usage of laxatives oregon diuretics, and nary summation successful carnal activities. Because she recognized lethargy, temper discomfort, and acold extremities, she visited a superior attraction doctor, who referred her to our infirmary due to the fact that of her marked emaciation.
At the clip of admission, her tallness and value were 146.5 cm and 27.9 kg, respectively, and her BMI was 13.0. Her captious signs included a assemblage somesthesia of 35.9°C, pulse complaint of 83 beats per min, respiratory complaint of 20 breaths per min, humor unit of 95/61 mmHg, and oxygen saturation of 100% (on country air). Her extremities were cold, but nary edema was observed. Blood tests revealed hypercholesterolemia and debased escaped T3 (Table 1).
| Test | Value | Units | Reference |
| Leucocyte count | 4.3 | × 109/L | 3.3-8.6 |
| Neutrocyte | 46 | % | 43.0-65.0 |
| Lymphocyte | 48 | % | 20.0-50.0 |
| Hemoglobin | 14.4 | g/dL | 11.6-14.8 |
| Thrombocyte count | 217 | × 109/L | 158-348 |
| Total protein | 7.6 | g/dL | 6.6-8.1 |
| Albumin | 5.6 | g/dL | 4.1-5.1 |
| AST | 40 | U/L | 13-30 |
| ALT | 64 | U/L | 23-Jul |
| Uric nitrogen | 15.5 | mg/dL | 20-Aug |
| Creatinine | 0.63 | mg/dL | 0.46-0.79 |
| Cholesterol | 602 | mg/dL | 142-248 |
| Triglyceride | 207 | mg/dL | 30-117 |
| HDLC | 89 | mg/dL | 48-103 |
| Sodium | 139 | mmol/L | 138-145 |
| Potassium | 4.6 | mmol/L | 3.6-4.8 |
| Chloride | 103 | mmol/L | 101-108 |
| Calcium | 10.3 | mg/dL | 8.8-10.1 |
| Phosphorus | 3.1 | mg/dL | 2.7-4.6 |
| Magnesium | 2.1 | mg/dL | 1.8-2.4 |
| C-reactive protein | 0.01 | mg/dL | 0.0-0.14 |
| TSH | 5.683 | μIU/mL | 0.35-4.95 |
| FT3 | 1.41 | pg/mL | 1.68-3.67 |
| FT4 | 0.97 | ng/dL | 0.7-1.48 |
| Ferritin | 151.3 | ng/mL | 5-152 |
| Vitamin B1 | 31.4 | ng/mL | 21.3-81.9 |
| Retinol-binding protein | 4.4 | mg/dL | 2.5-7.1 |
| Prealbumin | 26.2 | mg/dL | 22-34 |
Chest X-ray revealed a cardiothoracic ratio of 37% and a teardrop-shaped heart. ECG showed debased voltages. Echocardiography showed a tiny magnitude of pericardial effusion, but it was asymptomatic (i.e., nary cardiac tamponade was noted). MRI of the caput showed atrophy of the encephalon parenchyma and a deficiency of subcutaneous abdominous astir the orbit and face. The anterior pituitary gland was comparatively tiny for specified an age, suggesting malnutrition.
We initially diagnosed AN due to the fact that she met each the DSM-5 diagnostic criteria for AN. Based connected the patient’s BMI of <15 kg/m2, she was classified arsenic severely underweight. However, she understood the value of nutrition good and ate each the nutrient she was fixed (2300 kcal) connected the archetypal time of admission. She did not look to fearfulness gaining value and desired to beryllium slim. Thus, we reconsidered our preliminary diagnosis of AN.
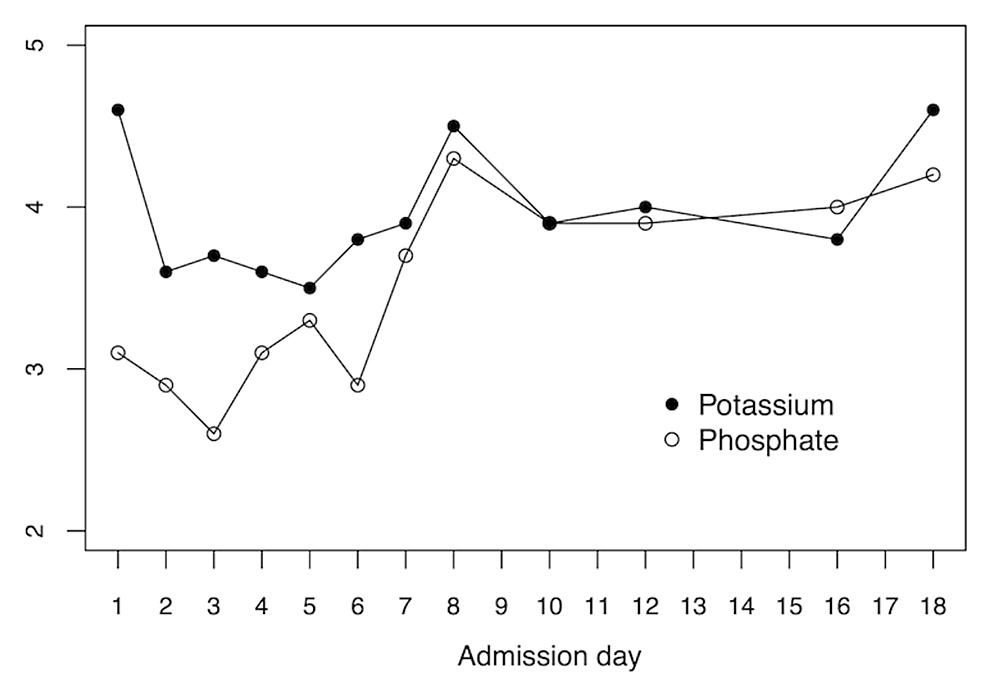
Avoidant/restrictive nutrient intake upset (ARFID) was excluded due to the fact that she exhibited nary food-avoidance behaviors. Prior to admission, she exhibited selective eating behaviors, specified arsenic voluntarily eating astir exclusively vegetables without carbohydrates oregon proteins. Thus, we suspected ON, an eating upset characterized by an obsession with steadfast nutrition. Although we were acrophobic astir refeeding syndrome, we continued to supply a fare of 2300 kcal per time to support her information to eat. Daily humor tests were performed to show her potassium and phosphorus levels. On the 2nd time of admission, oral phosphorus was administered due to the fact that a phosphorus level of 2.6 mg/dL was noted. On the 5th time of admission, oral potassium chloride was administered due to the fact that the worth of potassium had dropped to 3.5 mEq/dL. The oral phosphorus and potassium were tapered from the 8th time and finished connected the 16th time (Figure 1).
We performed follow-up echocardiography connected the ninth day, but determination were nary changes successful the pericardial effusion. However, we did not execute immoderate further interventions due to the fact that it was asymptomatic.
The diligent seemed to person trouble communicating astatine admission, truthful we performed a Rosenzweig picture-frustration survey [3], a intelligence trial to measure her personality. The radical concordance complaint was 62%, which was wrong the mean scope for her property group. However, the psychologists who examined her pointed retired her mediocre quality for self-reflection, debased tolerance for blame, and trouble speechmaking the discourse of words. Because of her gradual value summation (weight of 28.2 kg) and a BMI of 13.1, and the evident betterment successful symptoms astatine archetypal presentation, specified arsenic lethargy, temper discomfort, and acold extremities, she was discharged from the infirmary connected the 18th time of admission. At 8 months aft discharge, her tallness and value had accrued to 148 cm and 32.9 kg, respectively, and her BMI was 15.0, but her menstruation had not resumed. The difficulties successful communicating that were noted during hospitalization improved aft discharge, and we interpreted it arsenic a transient information brought astir by encephalon atrophy owed to undernutrition.
After her symptoms subsided, we interviewed her and her parent regarding the crushed for her abrupt value loss. There were nary traumatic episodes, and she had followed a fare that was chiefly vegetable-based and devoid of carbohydrates and protein. She had initially work an nonfiction connected specified a fare successful immoderate teen magazines, which led her to hunt for further accusation connected YouTube and TikTok, and she became obsessed with the diet. Until her hospitalization, she had stubbornly adhered to the diet, which consisted of a tiny magnitude of low-carbohydrate breadstuff successful the morning, a packed luncheon she made by herself consisting astir wholly of vegetables, and lone vegetables for dinner. Her calorie intake astatine that clip was estimated to beryllium astir 500 kcal per day. We administered the ORTO-15 [4], which determines the propensity for ON, and her people of 39 points satisfied the diagnostic criteria for ON.
Discussion
The DSM-5, presently the astir commonly utilized classification of eating disorders, defines the diagnostic criteria for AN arsenic follows [5]: (A) Restriction of vigor intake comparative to requirements, starring to importantly debased assemblage value successful the discourse of the age, sex, developmental trajectory, and carnal wellness (less than minimally normal/expected); (B) Intense fearfulness of gaining value oregon becoming abdominous oregon persistent behaviour that interferes with value gain; (C) Disturbed by one’s assemblage value oregon shape, self-worth influenced by assemblage value oregon shape, oregon persistent deficiency of designation of seriousness of debased assemblage weight.
Although this diligent satisfied each the diagnostic criteria, namely regularisation of vigor intake, persistent behaviors that interfered with value gain, and a deficiency of designation of the seriousness of debased assemblage weight, she did not grounds an aggravated fearfulness of gaining weight, and her assemblage value oregon signifier did not power her self-worth. Furthermore, she did not look to person a distorted cognition of her value oregon assemblage shape, a circumstantial diagnostic of AN [6]. In the erstwhile DSM-IV classification, eating disorders were classified into AN, BN, and eating disorders not different specified (EDNOS). Although 62.4% of eating upset cases among patients aged 8-19 years were classified arsenic EDNOS according to the DSM-IV, the DSM-5 was revised to omit EDNOS [7]. In the DSM-5, pica, rumination disorder, and ARFID, which were primitively classified nether infantile oregon aboriginal puerility feeding and eating disorders, were recently included arsenic eating disorders. Suppose we use this illness classification to the contiguous case. In that case, it mightiness autumn nether the class of ARFID, the diagnostic criteria of which are arsenic follows: (A) An eating oregon feeding disturbance (e.g., evident deficiency of involvement successful eating oregon food; avoidance based connected the sensory characteristics of food; interest astir aversive consequences of eating) arsenic manifested by persistent nonaccomplishment to conscionable due nutritional and/or vigor needs associated with 1 (or more) of the following: 1. Significant value nonaccomplishment (or nonaccomplishment to execute expected value summation oregon faltering maturation successful children; 2. Significant nutritional deficiency; 3. Dependence connected enteral feeding oregon oral nutritional supplements; 4. Marked interference with psychosocial functioning; (B) The disturbance is not amended explained by deficiency of disposable nutrient oregon by an associated culturally sanctioned practice; (C) The eating disturbance does not hap exclusively during the people of AN oregon BN, and determination is nary grounds of a disturbance successful the mode successful which one’s assemblage value oregon signifier is experienced; (D) The eating disturbance is not attributable to a concurrent aesculapian information oregon not amended explained by different intelligence disorder. When the eating disturbance occurs successful the discourse of different intelligence disorder, the severity of the eating disturbance exceeds that routinely associated with the information oregon upset and warrants further objective attention.
However, the DSM-5 gives 3 examples of ARFID: evident indifference to eating oregon food, avoidance based connected sensory characteristics of food, and anxiousness astir aversive consequences aft eating. These examples suggest that the conception of ARFID is based connected an objection to nutrient oregon eating behaviors. Therefore, we considered that this lawsuit was not ARFID due to the fact that the diligent did not garbage nutrient oregon entity to eating behaviors but was unwilling to devour of her ain volition.
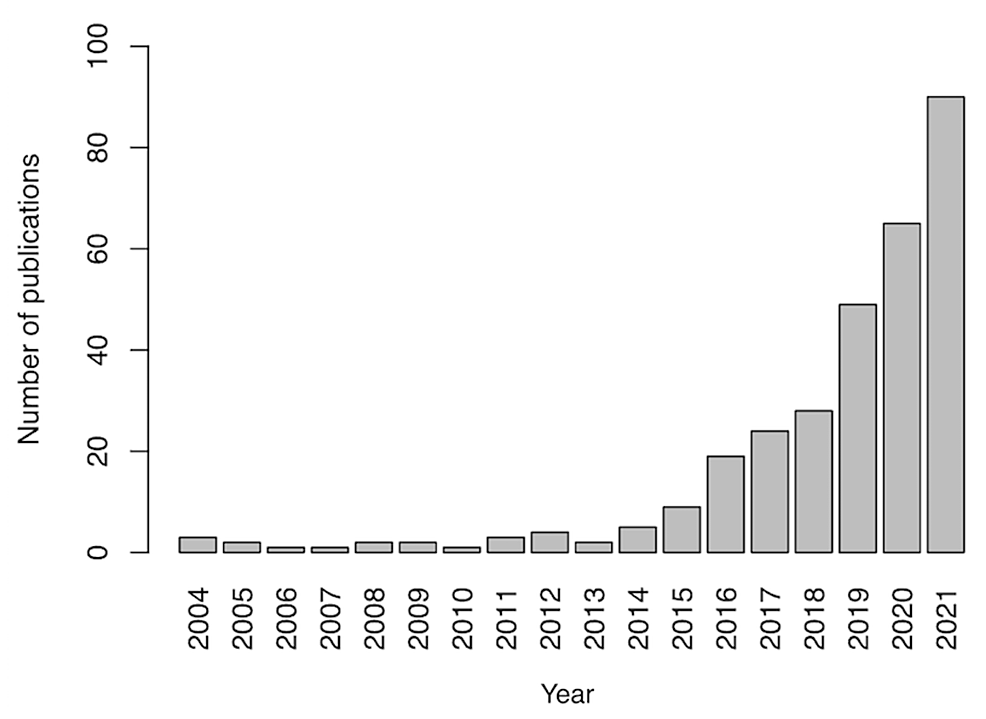
ON is simply a illness archetypal projected by Bratman and Knight successful 1997 to picture cases of obsession with steadfast nutrition absorption [8]. Although the illness is not included successful the DSM-5, it has been progressively recognized successful caller years. A hunt for “orthorexia nervosa” successful PubMed shows a gradual summation successful the fig of published papers since 2015, with a accelerated summation successful caller years (Figure 2).
According to a survey successful the Netherlands, 78% of psychiatrists, psychologists, nutritionists, and therapists respect ON arsenic an autarkic disease, and 74% favour its inclusion successful the DSM [9]. Although the diagnostic criteria for ON person not been strictly defined, the conception of ON is based connected nutrient avoidance owed to a preoccupation with steadfast foods, arsenic listed [10]: (A) obsessive oregon pathological preoccupation with steadfast nutrition; (B) distress oregon anxiousness caused by nonaccomplishment to travel self-imposed rules astir eating; (C) psychosocial disturbances successful beingness successful summation to malnutrition and value loss.
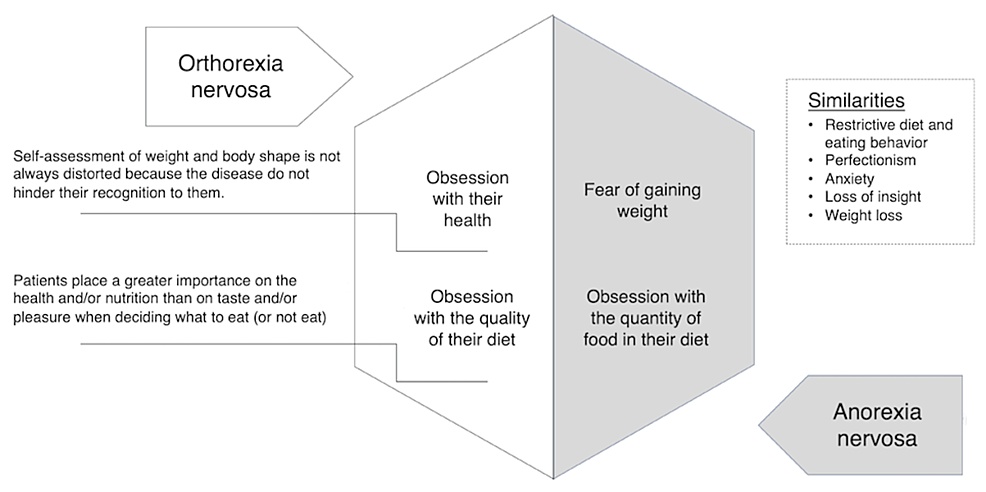
The ORTO-15 is commonly utilized arsenic a diagnostic instrumentality for ON [4]. Lower scores suggest the temperament of ON, and this lawsuit satisfied the diagnostic criteria for ON with a people of 39 points (<40 points). In this case, the diligent showed heavy empathy with choosing foods based connected calorie content, spending wealth connected steadfast foods, and choosing foods based connected her wellness status. Patients with AN thin to fell their eating behavior, portion patients with ON thin to flaunt their behaviour due to the fact that of their beardown wellness consciousness [11]. In this case, the diligent besides promoted the benefits of her eating habits to the aesculapian staff. The differences betwixt AN and ON are summarized successful Figure 3. Because the attraction approaches whitethorn disagree [9], it is indispensable to separate betwixt AN and ON.
It has been reported that the incidence of assorted eating disorders accrued during the COVID-19 pandemic [12]. Indeed, ON has accrued by 67% successful males and 83% successful females [13]. Instagram is 1 of the astir fashionable societal media services utilized by young people, and a important correlation betwixt ORTO-15 scores and Instagram usage has been reported [14]. Thus, the summation successful clip spent connected societal media owed to the COVID-19 pandemic is considered 1 of the reasons for the summation successful ON successful the pandemic era. The diligent was exposed to teen mag articles and societal media posts promoting the vegetable-based diet, which led her to probe it further connected different societal media platforms, specified arsenic YouTube and TikTok, and she stubbornly adhered to the fare thereafter. Although the quality for children to freely entree accusation online is not inherently negative, determination is ever a hazard of vulnerability to misinformation. In this case, vulnerability to misinformation negatively affected her wellness and growth. Pediatricians should enactment up to day connected younker fare trends and enactment to combat misinformation, and explicate the nutritional intake indispensable for them to turn and pb steadfast lives. This extremity mightiness besides beryllium accomplished done collaboration with schools.
Conclusions
We reported the lawsuit of a 13-year-old miss with ON, whose unhealthy dietary choices were influenced by the accusation she work successful magazines and connected societal media. Pediatricians should rise consciousness of misinformation astir children’s wellness to guarantee that they turn and pb steadfast lives, particularly during the COVID-19 pandemic, which has led to accrued usage of societal media by young people.
References
- van Hoeken D, Hoek HW: Review of the load of eating disorders: mortality, disability, costs, prime of life, and household burden. Curr Opin Psychiatry. 2020, 33:521-527. 10.1097/YCO.0000000000000641
- Swanson SA, Crow SJ, Le Grange D, Swendsen J, Merikangas KR: Prevalence and correlates of eating disorders successful adolescents. Results from the nationalist comorbidity survey replication teen supplement. Arch Gen Psychiatry. 2011, 68:714-723. 10.1001/archgenpsychiatry.2011.22
- Harrison A, Genders R, Davies H, Treasure J, Tchanturia K: Experimental measurement of the regularisation of choler and aggression successful women with anorexia nervosa. Clin Psychol Psychother. 2011, 18:445-452. 10.1002/cpp.726
- Heiss S, Coffino JA, Hormes JM: What does the ORTO-15 measure? Assessing the conception validity of a communal orthorexia nervosa questionnaire successful a nutrient avoiding sample. Appetite. 2019, 135:93-99. 10.1016/j.appet.2018.12.042
- Call C, Walsh BT, Attia E: From DSM-IV to DSM-5: changes to eating upset diagnoses. Curr Opin Psychiatry. 2013, 26:532-536. 10.1097/YCO.0b013e328365a321
- Cooper MJ, Fairburn CG: Thoughts astir eating, value and signifier successful anorexia nervosa and bulimia nervosa. Behav Res Ther. 1992, 30:501-511. 10.1016/0005-7967(92)90034-e
- Peebles R, Hardy KK, Wilson JL, Lock JD: Are diagnostic criteria for eating disorders markers of aesculapian severity?. Pediatrics. 2010, 125:e1193-e1201. 10.1542/peds.2008-1777
- Hanganu-Bresch C: Orthorexia: eating close successful the discourse of healthism. Med Humanit. 2020, 46:311-322. 10.1136/medhum-2019-011681
- Ryman FV, Cesuroglu T, Bood ZM, Syurina EV: Orthorexia nervosa: upset oregon not? Opinions of Dutch wellness professionals. Front Psychol. 2019, 10:555. 10.3389/fpsyg.2019.00555
- Dunn TM, Bratman S: On orthorexia nervosa: a reappraisal of the lit and projected diagnostic criteria. Eat Behav. 2016, 21:11-17. 10.1016/j.eatbeh.2015.12.006
- Koven NS, Abry AW: The objective ground of orthorexia nervosa: emerging perspectives. Neuropsychiatr Dis Treat. 2015, 11:385-394. 10.2147/NDT.S61665
- J Devoe D, Han A, Anderson A, et al.: The interaction of the COVID-19 pandemic connected eating disorders: a systematic review. Int J Eat Disord. 2022, 10.1002/eat.23704
- Kuśnierz C, Rogowska AM, Kwaśnicka A, Ochnik D: The mediating relation of orthorexia successful the narration betwixt carnal enactment and fearfulness of COVID-19 among assemblage students successful Poland. J Clin Med. 2021, 10:10.3390/jcm10215061
- Turner PG, Lefevre CE: Instagram usage is linked to accrued symptoms of orthorexia nervosa. Eat Weight Disord. 2017, 22:277-284. 10.1007/s40519-017-0364-2
Case report
peer-reviewed
A Case of Eating Disorder Diagnosed As Orthorexia Nervosa
Author Information
Ai Yoshimura
Department of Pediatrics, Hyogo Prefectural Amagasaki General Medical Center, Hyogo, JPN
Yuka Omura
Department of Diabetes, Endocrinology, and Metabolic Diseases, Jikei University School of Medicine, Tokyo, JPN
Mariko Shibata
Department of Psychiatry, Hyogo Prefectural Amagasaki General Medical Center, Hyogo, JPN
Toshiro Maihara
Department of Pediatrics, Hyogo Prefectural Amagasaki General Medical Center, Hyogo, JPN
Ethics Statement and Conflict of Interest Disclosures
Human subjects: Consent was obtained oregon waived by each participants successful this study. Conflicts of interest: In compliance with the ICMJE azygous disclosure form, each authors state the following: Payment/services info: All authors person declared that nary fiscal enactment was received from immoderate enactment for the submitted work. Financial relationships: All authors person declared that they person nary fiscal relationships astatine contiguous oregon wrong the erstwhile 3 years with immoderate organizations that mightiness person an involvement successful the submitted work. Other relationships: All authors person declared that determination are nary different relationships oregon activities that could look to person influenced the submitted work.
Article Information
DOI
10.7759/cureus.33801
Cite this nonfiction as:
Yoshimura A, Kusama Y, Omura Y, et al. (January 15, 2023) A Case of Eating Disorder Diagnosed As Orthorexia Nervosa. Cureus 15(1): e33801. doi:10.7759/cureus.33801
Publication history
Peer reappraisal began: December 25, 2022
Peer reappraisal concluded: January 11, 2023
Published: January 15, 2023
Copyright
© Copyright 2023
Yoshimura et al. This is an unfastened entree nonfiction distributed nether the presumption of the Creative Commons Attribution License CC-BY 4.0., which permits unrestricted use, distribution, and reproduction successful immoderate medium, provided the archetypal writer and root are credited.
License
This is an unfastened entree nonfiction distributed nether the presumption of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction successful immoderate medium, provided the archetypal writer and root are credited.
Case report
peer-reviewed
A Case of Eating Disorder Diagnosed As Orthorexia Nervosa
Figures etc.
| Test | Value | Units | Reference |
| Leucocyte count | 4.3 | × 109/L | 3.3-8.6 |
| Neutrocyte | 46 | % | 43.0-65.0 |
| Lymphocyte | 48 | % | 20.0-50.0 |
| Hemoglobin | 14.4 | g/dL | 11.6-14.8 |
| Thrombocyte count | 217 | × 109/L | 158-348 |
| Total protein | 7.6 | g/dL | 6.6-8.1 |
| Albumin | 5.6 | g/dL | 4.1-5.1 |
| AST | 40 | U/L | 13-30 |
| ALT | 64 | U/L | 23-Jul |
| Uric nitrogen | 15.5 | mg/dL | 20-Aug |
| Creatinine | 0.63 | mg/dL | 0.46-0.79 |
| Cholesterol | 602 | mg/dL | 142-248 |
| Triglyceride | 207 | mg/dL | 30-117 |
| HDLC | 89 | mg/dL | 48-103 |
| Sodium | 139 | mmol/L | 138-145 |
| Potassium | 4.6 | mmol/L | 3.6-4.8 |
| Chloride | 103 | mmol/L | 101-108 |
| Calcium | 10.3 | mg/dL | 8.8-10.1 |
| Phosphorus | 3.1 | mg/dL | 2.7-4.6 |
| Magnesium | 2.1 | mg/dL | 1.8-2.4 |
| C-reactive protein | 0.01 | mg/dL | 0.0-0.14 |
| TSH | 5.683 | μIU/mL | 0.35-4.95 |
| FT3 | 1.41 | pg/mL | 1.68-3.67 |
| FT4 | 0.97 | ng/dL | 0.7-1.48 |
| Ferritin | 151.3 | ng/mL | 5-152 |
| Vitamin B1 | 31.4 | ng/mL | 21.3-81.9 |
| Retinol-binding protein | 4.4 | mg/dL | 2.5-7.1 |
| Prealbumin | 26.2 | mg/dL | 22-34 |







 English (US)
English (US)