Introduction: Abdominal aortic aneurysms (AAA) person a varied presentation, which often makes the diagnosis difficult. The astir communal determination for an AAA is successful the infra-renal oregon distal aorta, which tin beryllium hard to visualize utilizing bedside ultrasound.
Objective: This survey was designed to place if a patient’s weight, gender, oregon property influenced our quality to visualize the distal aorta connected bedside abdominal aortic ultrasound scans.
Methods: All aortic scans completed successful the Emergency Department (ED) from September 2010 to September 2013 were retrospectively evaluated. Patients 21 years and older were included. Scans missing age, gender, oregon self-reported value were excluded.
Results: 500 aortic scans were included. The distal aorta was visualized successful 393 scans (78.6%). The mid aorta was visualized successful 417 scans (83.4%). The proximal aorta was visualized successful 454 scans (90.8%). For the distal aorta, the mean value for visualized versus not visualized was 75.7 kg versus 79.7 kg. For the proximal aorta, the mean value for visualized versus not visualized was 75.8 kg versus 84.0 kg. Weight importantly predicted the quality to visualize the proximal aorta (unadjusted p=0.0098, adjusted p=0.0095) and marginally predicted the quality to visualize the distal aorta (unadjusted p=0.071, adjusted p=0.019). Neither property (unadjusted p=0.13, adjusted p=0.052) nor sex (unadjusted p=0.74, adjusted p=0.40) was importantly associated with visualization.
Conclusion: There is nary clinically important quality successful the quality to visualize a patient’s distal aorta with bedside ultrasound based connected a patient’s assemblage weight, gender, oregon age.
Introduction
Developing an abdominal aortic aneurysm (AAA) is not uncommon, with the beingness hazard of being diagnosed with an AAA astir 1 successful 17 for the wide colonisation and astir 1 successful 9 for existent smokers [1,2]. The diligent presumption of a AAA tin vastly vary, making it a hard diagnosis [3,4]. Few patients with AAA oregon ruptured AAA contiguous with the classical triad of abdominal pain, hypotension, and pulsatile wide [1,4-9]. Therefore, the diagnosis of a AAA whitethorn beryllium missed oregon delayed, with perchance disastrous results [3,4,10-12]. Moreover, astir 33% of patients bash not cognize that they person an AAA [13], with 1 root citing implicit 80% of AAA lacking a erstwhile diagnosis erstwhile the aortic rupture occurred [3]. Ruptured AAAs person a mortality complaint adjacent to 90% [3,4,7,14,15].
Ultrasound has been utilized for galore years arsenic an adjunct to the diagnosis of AAA, particularly arsenic an outpatient screening exam [1,5]. Additionally, successful patients with a known AAA, ultrasound is often utilized to show the size progression of the aneurysm [5,14]. For symptomatic patients successful the exigency section (ED), the bedside ultrasound has go an indispensable instrumentality successful establishing oregon excluding the diagnosis of a AAA [1,3,6,15,16]. In an undifferentiated patient, bedside ultrasound is particularly utile to statesman searching for the diagnosis successful a critically ill, hemodynamically unstable patient. Although computed tomography (CT) is inactive required to find if the AAA is leaking, the beingness of symptoms and dilated aorta connected ultrasound is typically capable to suggest a affirmative diagnosis and expedite surgical consultation and attraction [4].
While usage is operator-dependent, ED physicians with constricted AAA ultrasound grooming tin place AAA successful patients with astir 100% accuracy [17]. Bedside ultrasound is astir 100% delicate and circumstantial for diagnosing AAAs [6,7]. Furthermore, bedside ultrasound was shown to beryllium comparable to accepted radiology ultrasound for the diagnosis of AAA [18]. Internal medicine residents who completed 4 one-on-one sessions connected the usage of ultrasound (US) to observe AAA were capable to place AAA successful patients with astir the aforesaid accuracy arsenic a credentialed sonographic teacher [19].
Patients of antithetic genders, races, and assemblage habitus acquisition bedside AAA ultrasound exams successful the ED. The astir communal determination for an AAA is the infra-renal (distal) aorta. While bedside ultrasound offers a unsocial mode to measure for AAA, diligent characteristics whitethorn bounds the quality to get a meaningful scan [6]. Because of assorted carnal attributes (body habitus, bowel gas, scars), the distal aorta tin beryllium particularly hard to visualize. In 1 radiology study, astir 33% of inconclusive abdominal ultrasounds demonstrated pathology successful follow-up CT scans [20]. Our superior extremity was to place if a patient’s value influenced the quality to visualize the aorta connected bedside abdominal aortic ultrasound scans. Our secondary extremity was to find if a patient’s sex influenced our quality to visualize the aorta connected bedside aortic ultrasounds.
This nonfiction was antecedently presented astatine the American College of Emergency Physicians Scientific Assembly Research Forum 2014.
Materials & Methods
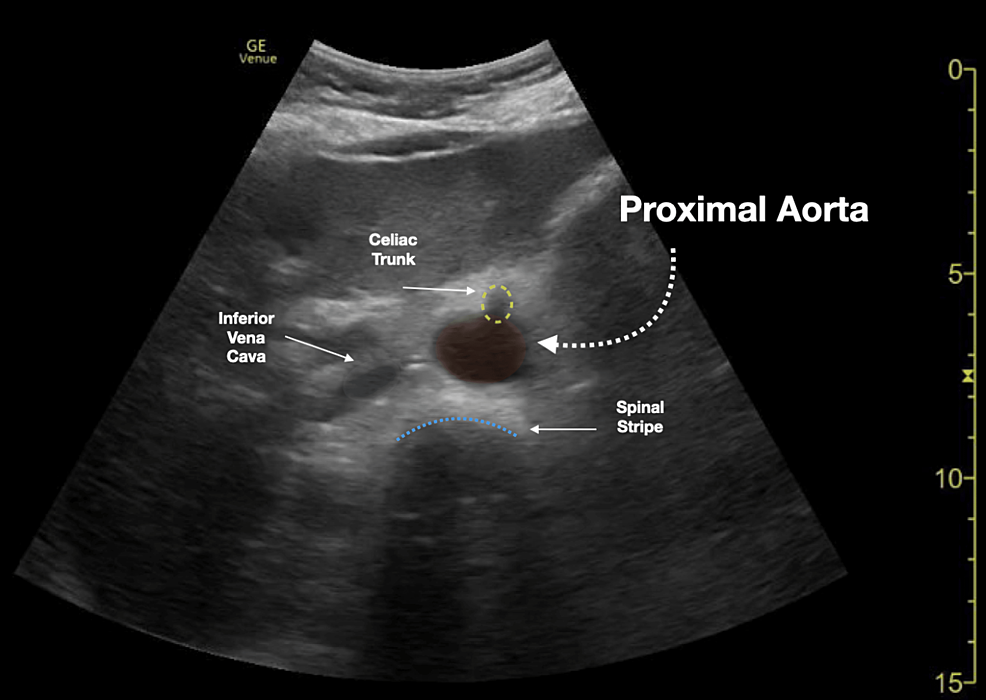
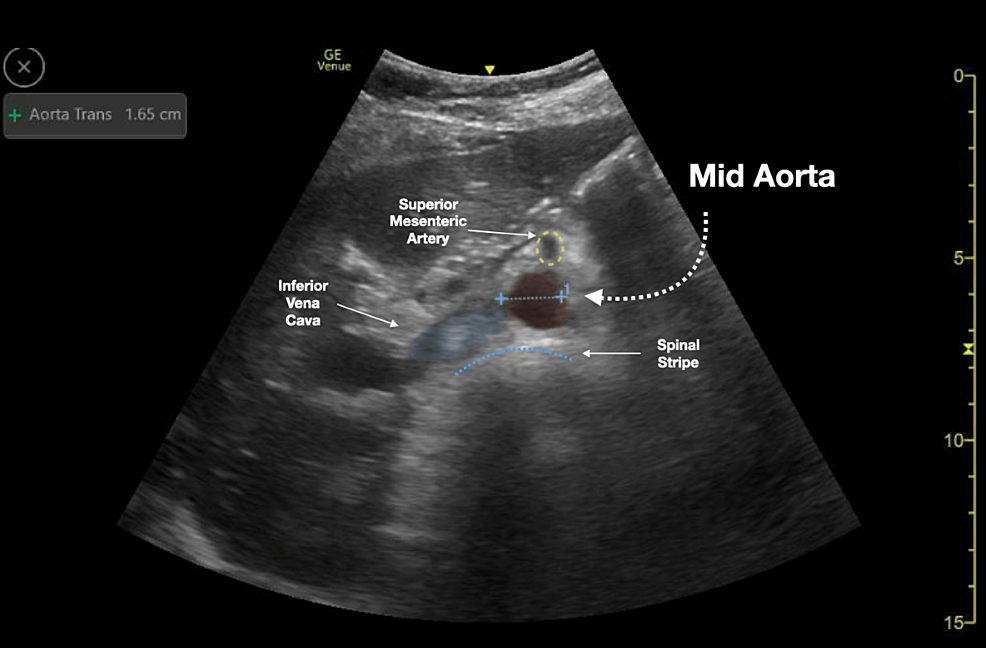
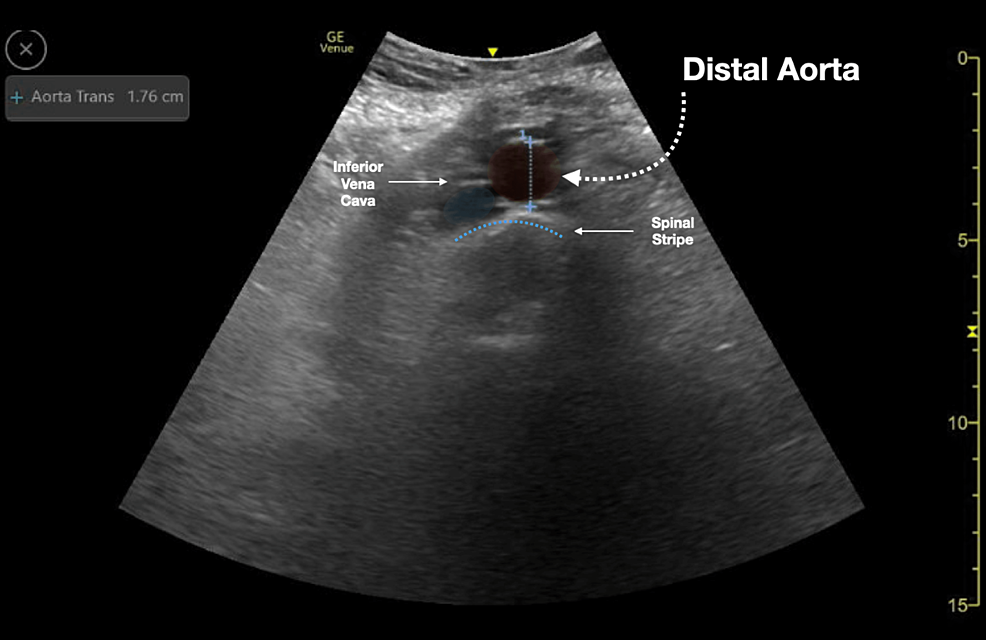
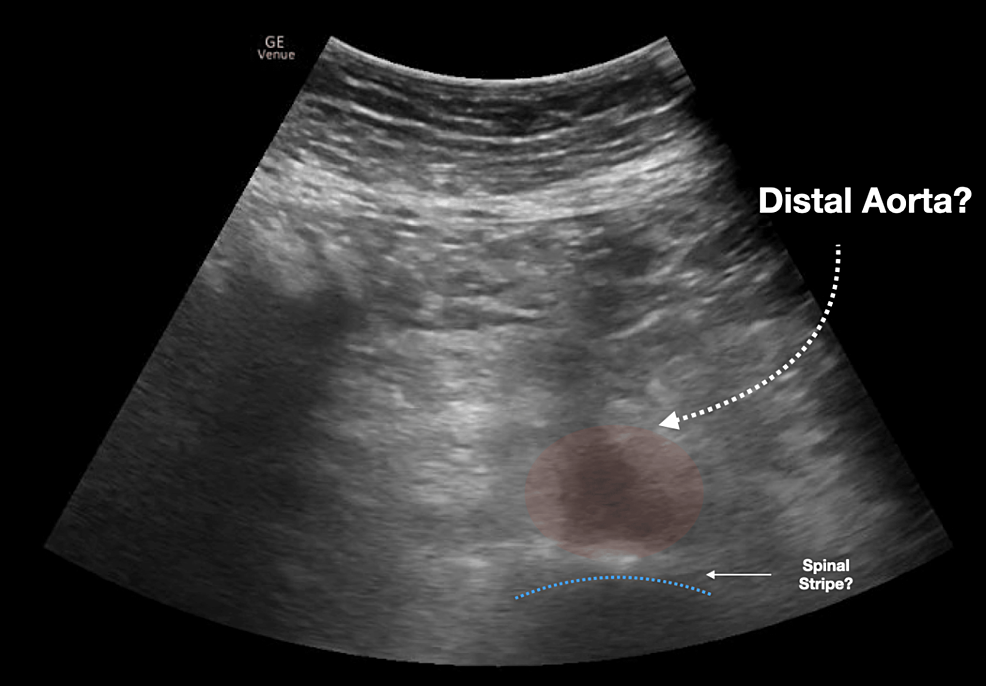
We conducted a retrospective illustration reappraisal of exigency section (ED) bedside aortic ultrasound scans completed astatine an world tertiary municipality level 1 trauma center. All aortic scans were completed successful the exigency section nether the supervision of qualified ED physicians and were recorded/stored successful a prime power database (Qpath © 2011 Telexy Healthcare, Inc.). Subsequently, a worksheet reviewing the scan and providing an mentation was completed by the idiosyncratic performing the bedside ultrasound. The worksheet and accompanying ultrasound images were reviewed by an exigency ultrasound fellowship-trained doc to guarantee the adequacy of scan interpretations. Though measurements of the aorta could beryllium taken astatine aggregate areas on the aorta, this survey focused connected whether the proximal, mid, and distal aorta was adequately visualized. Figures 1-3 show illustration ultrasound images of the proximal, mid, and distal aorta. In these images, the aorta and surrounding structures are easy identified and measured. On the different hand, Figure 4 shows an illustration of an ultrasound representation of the distal aorta, which is hard to intelligibly separate from surrounding structures.
A database of aortic scans betwixt September 2010 and September 2013 was extracted from the database, and the age, gender, and self-reported value were extracted from the physics aesculapian grounds by an unblinded reviewer. We included each patients 21 years and older who presented to the exigency section during the survey play and had a bedside abdominal aortic scan completed and reviewed successful Qpath. Patients beneath the property of 21, whose sex was unknown, oregon whose self-reported value was not recorded were excluded. Incomplete Qpath worksheets were besides excluded. All included aortic scans were already being completed for regular objective purposes. Scans were completed utilizing a Zonare (Z.One Ultra, Mountain View, CA) oregon Sonosite (M-Turbo, Bothell, Washington) device. All ED physicians had grooming connected the cognition of these ultrasound devices previously, enabling them to beryllium acquainted with their functions. The aesculapian school’s Institutional Review Board approved this study.
The means, modular deviations, and histograms were utilized to summarize the distributions of property and weight, portion frequencies summarized the distributions of sex and visualization of aortas. Logistic regression was utilized to measure the adjusted and unadjusted effects of weight, gender, and property connected visualization of the proximal, mid, and distal aorta.
Results
A full of 711 aortic scans were completed and recorded successful the database during the survey period. Of the 711 completed scans, 185 were excluded from the survey due to the fact that of incomplete worksheets. An further 26 scans were excluded due to the fact that age, gender, and value were inappropriately documented oregon missing. A full of 500 aortic scans were included. The mean diligent property was 67 ± 19 years. The mean value was 76.6 ± 20.1 kg. 264 males and 236 females were included successful the survey (Table 1). The distal aorta was adequately visualized successful 393 scans (78.6%). The mid aorta was adequately visualized successful 417 scans (83.4%). The proximal aorta was adequately visualized successful 454 scans (90.8%). The complaint of visualization was top for the proximal aorta, followed by the mid aorta, and lastly by the distal aorta (Table 2). The astir communal crushed cited for the non-visualization of immoderate portion of the aorta was the beingness of bowel gas. Other reasons for the non-visualization of the aorta were diligent noncompliance and instrumentality malfunction. The mean value of patients successful whom the distal aorta was adequately visualized was 75.7 kg, portion the mean value of patients successful whom the distal aorta was not adequately visualized was 79.7 kg (unadjusted p=0.071, adjusted 0.019). The mean value successful males for whom the distal aorta was adequately visualized and not adequately visualized was 81.0 kg and 84.9 kg, respectively. The mean value successful females for whom the distal aorta was adequately visualized and not adequately visualized was 69.7 kg and 74.1 kg, respectively. Weight importantly predicted visualization for the proximal aorta (unadjusted p=0.0098, adjusted p=0.0095) and was marginally associated with visualization of the distal aorta (unadjusted p=0.071, adjusted p=0.019). Neither property nor sex was importantly associated with the visualizations (Table 3). Additional analyses recovered that the effects of value oregon property connected visualization did not disagree importantly by sex (all p>0.20).
| Demographics | Included (N=500) Mean (SD) oregon N (%) | Excluded (N=170) Mean (SD) oregon N (%) | P-value |
| Age (Years) | 67.0 (18.5) | 58.1 (20.1) | <0.0001 |
| Weight (Kg) | 76.6 (19.8) | 80.5 (21.9) | 0.029 |
| Gender (Male) | 264 (52.8%) | 86 (50.6%) | 0.62 |
| Visualization of | Included (N=500) N (%) |
| Proximal Aorta | 454 (90.8%) |
| Mid Aorta | 417 (83.4%) |
| Distal Aorta | 393 (78.6%) |
| Aorta Visualized Mean (SD) oregon N (%) | P-value for Difference* | ||||
| Unadjusted | Adjusted+ | ||||
| Proximal Aorta | Yes (N=454) | No (N=46) | |||
| Age (Years) | 66.9 (18.4) | 68.0 (19.4) | 0.72 | 0.35 | |
| Weight (kg) | 75.8 (19.5) | 84.0 (21.8) | 0.0098 | 0.0095 | |
| Gender (Male) | 237 (52.2%) | 27 (58.7%) | 0.40 | 0.79 | |
| Mid Aorta | Yes (N=417) | No (N=83) | |||
| Age (Years) | 66.7 (18.4) | 68.9 (18.9) | 0.31 | 0.20 | |
| Weight (kg) | 76.1 (19.0) | 79.0 (23.6) | 0.22 | 0.16 | |
| Gender (Male) | 218 (52.3%) | 46 (55.4%) | 0.60 | 0.84 | |
| Distal Aorta | Yes (N=393) | No (N=107) | |||
| Age (Years) | 66.4 (18.7) | 69.4 (17.6) | 0.13 | 0.052 | |
| Weight (kg) | 75.7 (19.1) | 79.7 (22.2) | 0.071 | 0.019 | |
| Gender (Male) | 209 (52.2%) | 55 (51.4%) | 0.74 | 0.40 | |
Discussion
In the ED, patients get successful undifferentiated daze regularly. ED clinicians indispensable support a precocious objective suspicion for AAA successful patients with abdominal symptom and shock. The bedside ultrasound is simply a invaluable instrumentality due to the fact that these unstable patients tin beryllium kept wrong arm’s scope of captious attraction resources alternatively than sending them to the radiology department. Although ultrasound representation acquisition is relation dependent, adjacent the astir seasoned sonographer tin beryllium heard anecdotally questioning the feasibility of performing an abdominal aortic scan connected a diligent who is importantly overweight. The ultrasound relies connected the propagation of soundwaves to nutrient a ocular image. The further the representation is from the probe, the much apt the dependable waves volition beryllium scattered, producing an unreliable image, arsenic is the lawsuit with an obese idiosyncratic [21].
This survey demonstrates that though determination was a marginal quality successful the quality to visualize the distal aorta successful narration to value (75.7 kg visualized versus 79.7 kg unvisualized), this quality of 4 kg is comparatively tiny and apt to beryllium clinically ambiguous. Furthermore, the modular deviation was 19.1 kg for the radical wherever the distal aorta was visualized and 22.2 kg for the radical wherever the distal aorta was not visualized. Studies person examined the accuracy of diligent self-reported value and noted that patients are not wholly close successful reporting their value [22,23]. Therefore, fixed the overlap, value should not beryllium utilized to routinely exclude aortic scans.
In Table 1, the value of included versus excluded ultrasounds had a p-value of 0.029, presenting imaginable for quality betwixt populations included and excluded successful this study. Despite the p-value, the mean value quality betwixt the 2 groups is little than 4kg, making the tiny value quality look improbable to beryllium clinically relevant. The excluded scans included those with incomplete documentation.
The astir communal crushed for imaging inadequacy was the beingness of bowel gas, and this did not correlate to weight. Although the distal aorta was not visualized successful 21.4% of the patients included successful this study, the corollary is that bedside ultrasound imaging was adjuvant successful reducing contiguous interest for AAA successful 78.6% of patients. This enabled the ED clinician to re-evaluate their differential successful existent clip during the acute resuscitation signifier of the patient’s ED course. Thus, we urge that a patient’s value should not beryllium a contraindication to performing bedside abdominal aortic scans.
Limitations
We admit respective limitations successful this study. Our illustration size was comparatively small. While we were capable to analyse 500 scans, astir a 3rd of the illustration was excluded due to the fact that of incomplete documentation. As it tin beryllium hard to construe upon aboriginal reappraisal what information of the aorta was captured during the archetypal scan, studies without implicit documentation were excluded. While astir incomplete worksheets did not specifically remark connected what constricted their quality to visualize the aorta, factors different than aortic visualization could person contributed to their incomplete status. Given that the intent of this survey was to analyse if a value had immoderate power connected the quality to visualize the aorta, the deficiency of sonographer reasoning is simply a ample limitation. Clinicians of varying acquisition were included successful this study, and though each the scans were performed nether the supervision of a qualified sonographer and reviewed by an exigency ultrasound fellowship-trained physician, representation acquisition is inactive relation dependent. A enactment bias mightiness besides person been involved, fixed that determination was skepticism astir successfully obtaining an aortic scan connected overweight individuals, starring a clinician to either not execute oregon not grounds an abdominal ultrasound. Finally, the usage of 2 antithetic ultrasound devices was a regulation due to the fact that each instrumentality displays images differently, which whitethorn power the clinician’s quality to get images.
Conclusions
Bedside ultrasound is an important instrumentality successful helping to constrictive down the differential and diagnose AAAs, particularly successful critically sick ED patients. In a emblematic ED, diverseness exists among patients’ gender, assemblage habitus, and different characteristics. In this study, diligent weight, sex oregon property did not importantly clinically interaction the ultrasound operators’ quality to visualize the distal aorta. Based connected this study, a patient’s weight, gender, oregon property should not play a cardinal relation successful the exigency clinician’s determination to scan the distal aorta connected a bedside ultrasound.
- Kessler V, Klopf J, Eilenberg W, Neumayer C, Brostjan C: AAA revisited: A broad reappraisal of hazard factors, management, and hallmarks of pathogenesis. Biomedicines. 2022, 10:10.3390/biomedicines10010094
- Tang W, Yao L, Roetker NS, et al.: Lifetime hazard and hazard factors for abdominal aortic aneurysm successful a 24-year prospective survey (atherosclerosis hazard successful communities). Arterioscler Thromb Vasc Biol. 2016, 36:2468-77. 10.1161/ATVBAHA.116.308147
- Rubano E, Mehta N, Caputo W, Paladino L, Sinert R: Systematic review: Emergency section bedside ultrasonography for diagnosing suspected abdominal aortic aneurysm. Acad Emerg Med. 2013, 20:128-38. 10.1111/acem.12080
- Singh M, Koyfman A, Martinez JP: Abdominal vascular catastrophes. Emerg Med Clin North Am. 2016, 34:327-39. 10.1016/j.emc.2015.12.014
- Hellawell HN, Mostafa AM, Kyriacou H, Sumal AS, Boyle JR: Abdominal aortic aneurysms portion one: Epidemiology, presumption and preoperative considerations. J Perioper Pract. 2021, 31:274-80. 10.1177/1750458920954014
- Lech C, Swaminathan A: Abdominal aortic emergencies. Emerg Med Clin North Am. 2017, 35:847-67. 10.1016/j.emc.2017.07.003
- Diaz O, Eilbert W: Ruptured abdominal aortic aneurysm identified connected point-of-care ultrasound successful the exigency department. Int J Emerg Med. 2020, 13:25. 10.1186/s12245-020-00279-9
- Hahn B, Bonhomme K, Finnie J, Adwar S, Lesser M, Hirschorn D: Does a mean screening ultrasound of the abdominal aorta trim the likelihood of rupture successful exigency section patients?. Clin Imaging. 2016, 40:398-401. 10.1016/j.clinimag.2015.11.021
- Kiell CS, Ernst CB: Advances successful absorption of abdominal aortic aneurysm. Adv Surg. 1993, 26:73-98.
- Marston WA, Ahlquist R, Johnson G Jr, et al.: Misdiagnosis of ruptured abdominal aortic aneurysms. J Vasc Surg. 1992, 16:17-22. 10.1067/mva.1992.34344
- Hoffman M, Avellone JC, Plecha FR, et al.: Operation for ruptured abdominal aortic aneurysms: a community-wide experience. Surgery. 1982, 91:597-602.
- Hiatt JC, Barker WF, Machleder HI, Baker JD, Busuttil RW, Moore WS: Determinants of nonaccomplishment successful the attraction of ruptured abdominal aortic aneurysm. Arch Surg. 1984, 119:1264-8. 10.1001/archsurg.1984.01390230036008
- Law M: Screening for abdominal aortic aneurysms. Br Med Bull. 1998, 54:903-13. 10.1093/oxfordjournals.bmb.a011737
- Ernst CB: Abdominal aortic aneurysm. N Engl J Med. 1993, 328:1167-72. 10.1056/NEJM199304223281607
- Halsey-Nichols M, McCoin N: Abdominal symptom successful the exigency department: Missed diagnoses. Emerg Med Clin North Am. 2021, 39:703-17. 10.1016/j.emc.2021.07.005
- Shuman WP, Hastrup W Jr, Kohler TR, Nyberg DA, Wang KY, Vincent LM, Mack LA: Suspected leaking abdominal aortic aneurysm: usage of sonography successful the exigency room. Radiology. 1988, 168:117-9. 10.1148/radiology.168.1.3289085
- Kuhn M, Bonnin RL, Davey MJ, Rowland JL, Langlois SL: Emergency section ultrasound scanning for abdominal aortic aneurysm: accessible, accurate, and advantageous. Ann Emerg Med. 2000, 36:219-23. 10.1067/mem.2000.108616
- Lin PH, Bush RL, McCoy SA, et al.: A prospective survey of a hand-held ultrasound instrumentality successful abdominal aortic aneurysm evaluation. Am J Surg. 2003, 186:455-9. 10.1016/j.amjsurg.2003.07.018
- Riegert-Johnson DL, Bruce CJ, Montori VM, Cook RJ, Spittell PC: Residents tin beryllium trained to observe abdominal aortic aneurysms utilizing idiosyncratic ultrasound imagers: a aviator study. J Am Soc Echocardiogr. 2005, 18:394-7. 10.1016/j.echo.2004.12.019
- Gupta S, Saini S, Schultz T, et al.: Assessing the output of radiologists’ recommendations for further imaging pursuing equivocal abdominal ultrasound. Am Roentgen Ray Society Annual Meeting Abstracts. 2012, 046.
- Lagalla R, Midiri M: Image prime power successful bosom ultrasound. Eur J Radiol. 1998, 2:229-33. 10.1016/s0720-048x(98)00067-9
- Yoong SL, Carey ML, D'Este C, Sanson-Fisher RW: Agreement betwixt self-reported and measured value and tallness collected successful wide signifier patients: a prospective study. BMC Med Res Methodol. 2013, 13:38. 10.1186/1471-2288-13-38
- Babiarczyk B, Sternal D: Accuracy of self-reported and measured anthropometric information successful the inpatient population. Int J Nurs Pract. 2015, 21:813-9. 10.1111/ijn.12314






 English (US)
English (US)